- The costs of integrating violence against women and girls programming into health services will vary according to the setting, because it depends on the services already available, e.g. the extent of training of service providers in counseling and/or gender sensitivity, and whether the facility already has the capacity to provider appropriate post-sexual violence services, such as provision of emergency contraception, the collection of medical/forensic evidence (e.g. rape kits), STI and HIV testing, and post-exposure prophylaxis (PEP) for HIV/AIDS and treatment for STIs.
- The costs to be considered include the following start-up one-time costs. This list assumes that the normal equipment and supplies for basic sexual and reproductive health services are in place.
- Any remodeling of facilities that is needed to provide the necessary privacy, usually outfitting a private room for counseling, or a room dedicated solely to the constellation of post-rape services that is not marked to ensure client safety and confidentiality.
- Adaptation of screening tools and protocols, which might necessitate the time of a researcher to verify culturally appropriate language and ways to surmount cultural barriers to disclosure.
- Training of health providers to apply protocols and provide initial gender-sensitive, sympathetic counseling.
- Time of health sector staff to set up the appropriate linkages and referral systems with police, judiciary, and psycho-social services.
- For post-sexual violence services, coordination with the legal system demands medico- infrastructure and equipment, e.g. laboratories to take biological samples, and any other items stipulated by law or that may help provide evidence in a case.
- The following recurrent costs must be considered if the service is to be sustainable. These must be built into budgets. Some of the recurrent costs will be fixed, but others will vary according to the number of women expected to use the service. As community-based education campaigns raise awareness about violence against women and girls and women’s rights, the numbers of women using the service should increase steadily.
- If the facility sets up a special service for violence against women and girls that did not exist previously, there will be annual operating costs.
- Many services have added a psychologist to the team to provide counseling and serve as the main person helping to direct women and girls to other sectors and support services.
- The need for training and support of health personnel dealing with cases is ongoing, to avoid burnout and maintain quality of services.
- Given skills and time constraints of many of the health providers doing the initial screening, many services in the literature added psychologists to existing services. Given the human resource constraints of most public sector health services, it is difficult to provide these additional support services without additional funding. (Hainsworth & Zilhão, 2009)
- For resource poor settings low-cost alternatives are suggested when psychosocial support is lacking, such as peer support groups for women.
- If post-sexual violence services are added, the cost of any additional laboratory tests and standard treatments, supplies, and medicine (e.g. HIV PEP, emergency contraception, STI treatment) as well as the costs of gathering of evidence for the juridical system according to national standards.
Source: excerpted/adapted from: UNFPA. N.d. Addressing Violence Against Women and Girls in Sexual and Reproductive Health Services: A Review of Knowledge Assets, pgs.28-29.
Case Study: South Africa Costs Services to Provide Better Care for Sexual Assault Survivors
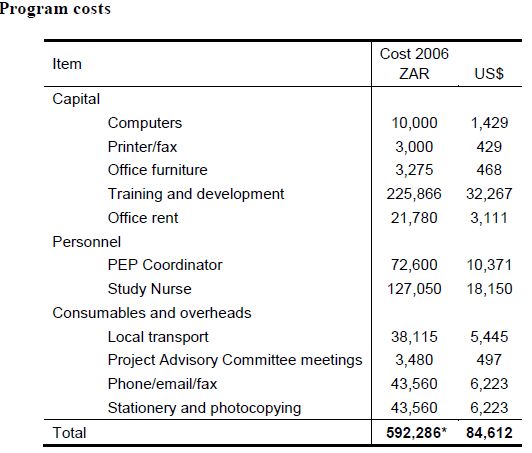
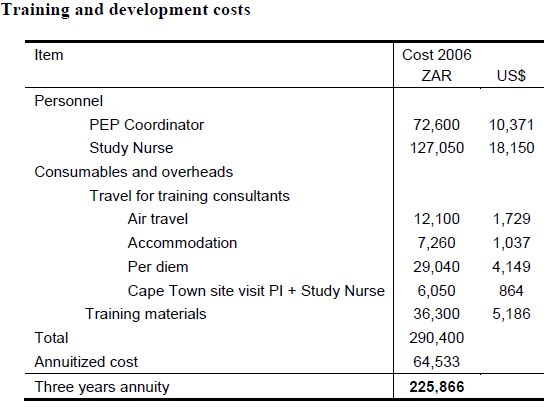
In South Africa, the following cost analysis measured the additional cost of strengthening the existing post-rape services. After conducting formative research, a five-part intervention model was introduced in a district hospital in rural South Africa. This intervention cost $84,612 over three years. The major cost items were the initial investment in training and development, and the salaries of the Post Exposure Prophylaxis Coordinator and Study Nurse. Thus, the routine service delivery costs (total costs minus initial training and development costs) were $52,345 (ZAR 366,420) over the three years, which translates into an estimated annual cost of $17,449 (ZAR 122,140).
The introduction of the model resulted in, among others: an increase in the volume of rape cases presenting to hospital (from 8 to 13 cases per month); improved efficiency of services with rape survivors; improved quality of services (e.g. exams, provision of pregnancy testing, emergency contraception, sexually transmitted infection treatment, voluntary counselling and testing, post exposure prophylaxis, counselling and referrals), and; an increased role for nurses.
The results of this study suggest that it is possible to improve comprehensive services for the medical management of sexual assault, including post-exposure prophylaxis within a public sector hospital, using existing staff and resources, and that with additional training, nurses can play an expanded role in this care. There have been few such studies conducted in an African setting, and the findings are important for understanding how the health system is currently coping with high levels of sexual violence in communities – and how they might be improved.
Source: excerpted/adapted from: Kim, J., et al., 2007a. Developing an Integrated Model for Post-Rape Care and HIV Post-Exposure Prophylaxis in Rural South Africa. Washington, D.C.: Population Council, Rural AIDS & Development Action Research Programme, School of Public Health, University of Witwatersrand, South Africa and Tshwaranang Legal Advocacy Centre, South Africa).
Illustrative Resources:
Gender Responsive Budgeting and Women’s Reproductive Rights: A Resource Pack (UNFPA and UNIFEM, 2006). Available in English, French and Spanish.
Gender Responsive Budgeting in Practice: A Training Manual (UNFPA and UNIFEM. 2006a). Available in English.
Hospital Costing Model Manual (Newbrander, W. and Lewis, E., 1999). Available in English.
